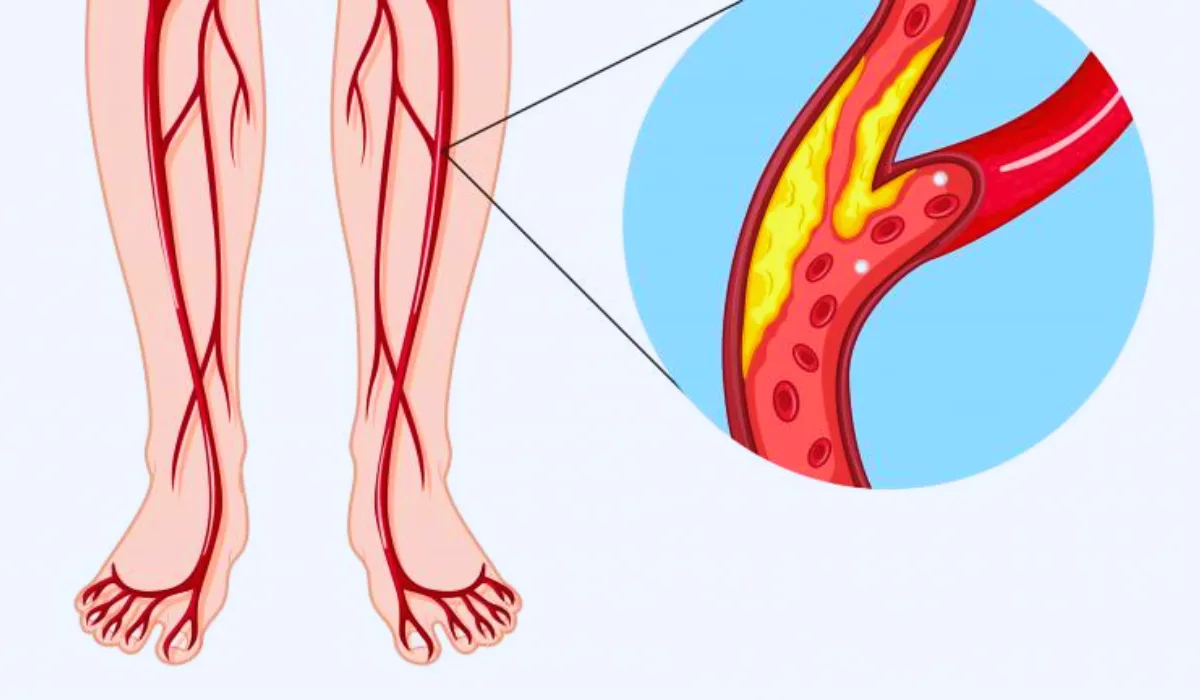
Peripheral Artery Disease (PAD) is a commonly yet often overlooked circulatory problem that affects millions of people worldwide. Characterized by narrowed arteries in the limbs, particularly the legs, PAD can lead to a range of symptoms, from leg pain during walking to more severe complications. The condition is primarily caused by atherosclerosis, where fatty deposits clog the arteries, restricting blood flow.
Awareness and understanding of PAD are critical, as early detection and management can significantly improve quality of life and prevent serious complications. Often underdiagnosed, PAD can be a red flag for other cardiovascular diseases.
In this blog, we will discuss symptoms, causes, and management strategies to overcome the effects of PAD.
Overview of Peripheral Artery Disease
It is a medical condition characterized by the narrowing of peripheral arteries, primarily in the legs, due to atherosclerotic plaque buildup. This plaque, composed of cholesterol, fat, and other substances, accumulates on the artery walls. This leads to reduced blood flow to the limbs.
It predominantly affects older adults, particularly those over the age of 65, with a higher prevalence among smokers and individuals with a history of hypertension, diabetes, or cardiovascular diseases.
Peripheral Artery Disease: Symptoms and Causes
Common symptoms of PAD include leg pain or cramping during activities like walking or climbing stairs, which typically subsides with rest. This condition, known as claudication, results from the muscles not receiving enough blood during exertion. However, many individuals with PAD may be asymptomatic or attribute their symptoms to aging. Several PADs can lead to non-healing wounds, changes in skin color, or decreased leg temperature.
The primary cause of PAD is atherosclerosis. Risk factors include smoking, high cholesterol, diabetes, obesity, high blood pressure, and sedentary lifestyle. Age and a family history of cardiovascular diseases also contribute to the risk.
Furthermore, individuals with higher PAD risk can develop coronary artery disease, heart attacks, or strokes, due to the underlying atherosclerosis affecting arteries throughout the body. This interconnection of vascular diseases underscores the need for comprehensive cardiovascular health management.
Diagnosis and Tests
Diagnosing Peripheral Artery Disease typically begins with a thorough medical history review and a physical examination. One key initial test is the Ankle-Brachial Index (ABI), a non-invasive test that compares the blood pressure in the ankle with the blood pressure in the arm. An ABI ratio lower than 1.0 is indicative of PAD. If PAD is suspected, further diagnostic tests include Duplex ultrasound, which uses high-frequency wave sounds to visualize the arterial blood flow and identify blockages or narrowing.
In some cases, more advanced imaging techniques like Magnetic Resonance Angiography (MRA) or Computerized Tomography Angiography (CTA) are used to obtain detailed images of the blood vessels. For a definitive diagnosis, an angiogram, which involves entering a contrast dye into the arteries and taking X-rays, may be performed.
These tests help confirm the diagnosis of PAD and determine the severity and treatment of this disease.
Management and Treatment
Managing PAD involves a combination of lifestyle changes, medication, and in some cases, surgical intervention. Lifestyle modifications are the cornerstone of PAD management, including smoking cessation, a healthy diet, and regular exercise. Structured exercise programs, particularly supervised exercise therapies, have shown significant benefits in improving symptoms and overall vascular health. Medications may be prescribed to manage risk factors such as high blood pressure, cholesterol, and diabetes, and to prevent blood clots as well.
In more severe cases, medical procedures may be necessary. Angioplasty, where a small balloon is inserted and inflated to open up the artery, or bypass surgery, which involves using a vessel from another part of the body to reroute blood around the blocked artery, are common surgical options.
Additionally, in cases of critical limb ischemia, procedures to restore blood flow are essential to prevent amputation. The management of PAD is a long-term process focusing on reducing symptoms, improving quality of life, and preventing disease progression and complications.
Prevention of PAD
Preventing PAD largely involves adopting a healthier lifestyle. Key modifications include quitting smoking, which is a significant risk factor for PAD, and maintaining a balanced diet rich in fruits, vegetables, and whole grains to reduce cholesterol levels. Regular physical activities like walking and cycling can improve circulation and overall vascular health. Managing underlying health conditions like hypertension, diabetes, and high cholesterol through medication and lifestyle changes is crucial.
Regular checkups and risk assessments are vital, especially for those with a family history of PAD or cardiovascular diseases. Early detection of risk factors and initiating preventive measures can significantly reduce the chances of developing PAD. It’s important to discuss with a healthcare provider about screening for PAD if you have symptoms or risk factors.
Read More: 10 Foods to Improve Athletic Performance
Conclusion
Awareness and management of Peripheral Artery Disease is crucial in preventing its progress and related complications. Understanding the symptoms, causes, and treatment options empowers individuals to seek timely medical advice.
Lifestyle modifications play a vital role in both prevention and management of PAD. Regular medical checkups and proactive health measures are crucial, especially for those at higher risk. Early detection and intervention can lead to better health outcomes, highlighting the importance of benign vigilant about vascular health.
FAQs
A1. Common symptoms include leg pain or cramping during physical activities, numbness or weakness in the legs, and changes in leg skin color or temperature. Some people might not experience any symptoms.
A2. Yes, PAD can increase the risk of coronary artery disease, heart attack, and stroke due to atherosclerosis affecting other arteries.
A3. Treatment options for PAD include lifestyle changes (like quitting smoking and exercising), medications to manage symptoms and risk factors, and in some cases, surgical procedures like angioplasty or bypass surgery.
A4. While not entirely preventable, lifestyle changes can significantly reduce the risk of developing PAD. This includes maintaining a healthy diet, regular exercise, and avoiding smoking.
A5. Yes, regular exercise can improve symptoms of PAD and overall vascular health.