Menopause is a natural transition in a woman’s life. It is marked by the cessation of the menstrual cycle. Many women go through vaginal dryness, which can cause discomfort and reduce the enjoyment of sexual pleasure. It’s a common condition but not openly discussed. It can cause considerable discomfort and frequently results in reduced enjoyment of sexual activities.
Moreover, it can profoundly affect a woman’s emotional health. Knowing the reasons for vaginal dryness is important. Recognizing its warning signs and knowing treatment options are vital steps. These steps may prove essential in enhancing the sexual wellness of postmenopausal women. This article provides an in-depth exploration of vaginal dryness during menopause, its causes, symptoms, and treatment.
What is Vaginal dryness?
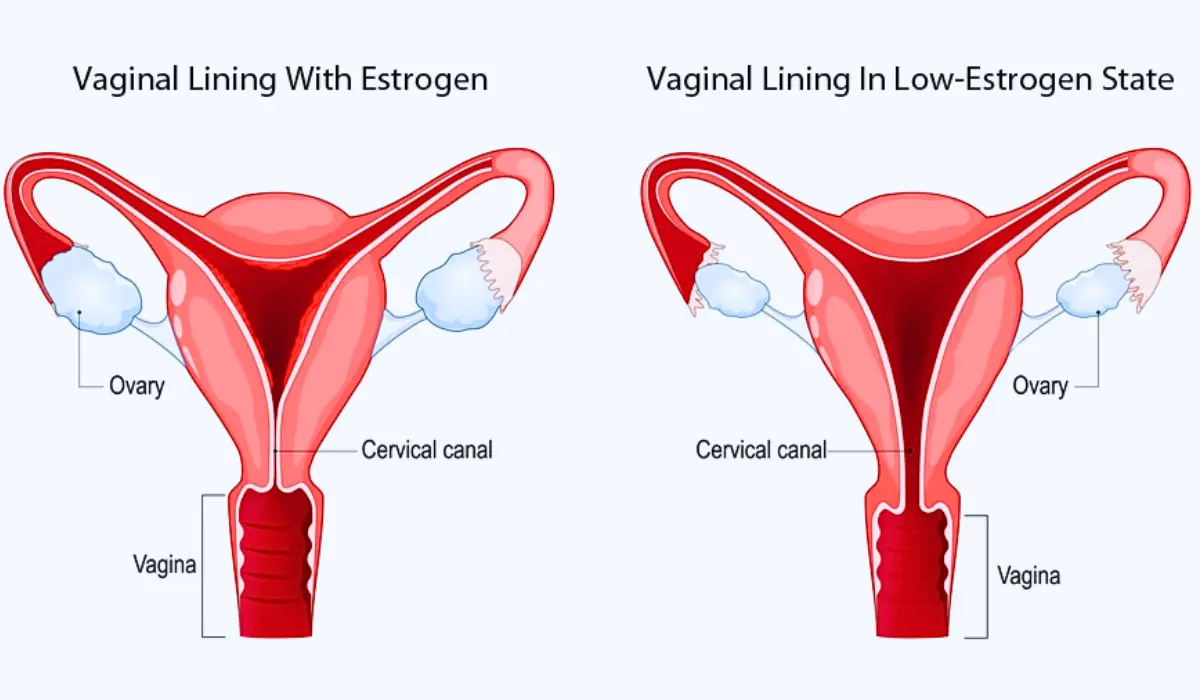
Vaginal dryness is widespread among women undergoing menopause. With dropping estrogen levels, vaginal tissue is thin and loses both elasticity and lubrication. This leads to uneasiness, itching, and irritation, especially during sex. Genitourinary syndrome of menopause (GSM) affects both the vaginal and urinary systems.
Causes of Vaginal Dryness After Menopause
After menopause, the leading cause of vaginal dryness is diminishing estrogen levels. Estrogen is a hormone that primarily maintains vaginal elasticity, and its reduced amount can highly affect vaginal health.
Hormonal Fluctuations And Perimenopause
Hormone levels fluctuate wildly during the transition to menopause. This change is also known as perimenopause, and it occurs before menopause, signaling the end of reproductive years. Many factors characterize Perimenopause:
Duration: Perimenopause mostly starts in a woman’s 40s, sometimes in her 30s, and can last about four years.
Hormonal changes: Ovaries make less estrogen during perimenopause, and the period becomes irregular. Decreased estrogen greatly affects a woman’s body and moods.
Symptoms: Typical signs of hormone level changes include:
- Irregular menstruation
- Hot flashes
- Sleep issues
- Mood swings
- Vaginal dryness
- Lower fertility
- Changes in sexual function
Physical changes: Shifting hormones can alter cholesterol, bone density, and heart health.
Fertility: Fertility drops in perimenopause, but pregnancy can still happen.
Diagnosis: Perimenopause is usually identified by signs like changes in period and hormone tests.
Other Contributing Factors
Besides hormone changes, several other factors can exacerbate vaginal dryness. These include Certain:
- Medications, such as antihistamines and antidepressants, which reduce overall body moisture, including the vaginal area. Smoking can also negatively influence blood circulation and cause vaginal dryness.
- Underlying health conditions can cause dryness, such as autoimmune disorders. One example is Sjögren’s syndrome.
How common is vaginal dryness?
Vaginal dryness is prevalent among women, particularly during menopausal transition. A study found that 19% of women aged 42-53 years reported vaginal dryness, rising to 34% in women aged 57-69 years. The increase is linked to women advancing through menopausal stages and surgical menopause.
Symptoms to Recognize:
The symptoms of vaginal dryness vary but typically include:
- You may experience Itching, burning, or soreness in the vaginal area
- Discomfort or pain during sexual intercourse
- A dry or tight feeling in the vaginal area.
- Light bleeding or spotting after intercourse
Recurring urinary tract infections can occur due to changes in vaginal health. Discomfort during urination is also possible because of this.
Impact on Sexual Health
Vaginal dryness can severely impact a woman’s sexual health. During intercourse, pain and discontent can cause people to avoid sexual activity. It can strain intimate relationships.
Diagnosis and Tests
A healthcare provider can diagnose vaginal dryness through:
- A doctor may take a pelvic exam to examine the vaginal walls and cervix.
- Discussion of aberrations and medical history.
- In some cases, tests rule out infections or other conditions that could be causing the issues.
Management and Treatment Options
Treatment for vaginal dryness includes a variety of options:
- Vaginal Estrogen Therapy: This is often the most effective treatment. You can get it in creams, tablets, or rings. You apply estrogen directly to the vaginal area.
- Oral Hormone Replacement Therapy (HRT): HRT is effective but carries risks. Discuss it with a healthcare provider.
- Lifestyle Modifications: To relieve symptoms, you can quit smoking, stay hydrated, and have an active sex life.
- Alternative Therapies: Some women explore natural remedies, such as herbal supplements or acupuncture. Talk to your doctor to ensure these options are safe.
Prevention and Lifestyle Change
To reduce the severity of vaginal dryness, consider the following:
- Avoiding irritants like scented soaps or douches
- Using lubricants during sexual intercourse.
- Regular sex or vaginal stimulation can help maintain vaginal health.
What helps with Vaginal Lubrication?
To help with vaginal dryness, people often use lubricants and moisturizers. Lubricants are good for making sex more comfortable. Lubricants ease friction and are found in different kinds: water-based ones are safe with condoms and easy to clean; silicone-based ones last longer and are good for use in water; and oil-based ones should not be used with latex condoms.
Moisturizers, different from lubricants, keep moisture for a long time, not just during sex. You can buy these products easily without a prescription. They help make sex better and more pleasurable for people with vaginal dryness.
When to see a Doctor?
When vaginal dryness affects your quality of life and makes you go through constant discomfort, itching, or pain, especially during sex, consult a doctor. It’s important to seek medical advice if other clinical signs accompany vaginal dryness, such as bleeding and unusual discharge. It may also include urinary problems, like frequent infections or incontinence.
These symptoms could indicate more severe conditions. If over-the-counter lubricants don’t work, a doctor can recommend other treatments. These may include hormonal therapies. Discuss vaginal dryness during routine gynecological check-ups, especially before or during menopause.
Conclusion
Vaginal dryness after menopause is a common yet controllable condition. Recognizing the problem early on can significantly enhance comfort and ease. Seeking appropriate treatment can greatly mitigate the Vaginal dryness issues. Open communication is vital in effectively handling this problem. Women can navigate this natural phase of life more comfortably. They can do this through a combination of medical treatments and lifestyle adjustments. Addressing vaginal dryness is important. It’s not just about physical health but it also preserves intimacy, confidence, and overall well-being in postmenopausal life.